Abstract
The rarity of Mixed-Phenotype Acute Leukemia (MPAL) and competing definitions has resulted in diffuse literature reporting small case series and precluded a consensus treatment approach. We therefore conducted a meta-analysis and systematic review to investigate the association of treatment type (acute lymphoblastic leukemia [ALL], acute myeloid leukemia [AML], or "hybrid" regimens) and disease response. We searched seven databases from inception through 2017 without age or language restriction. Included studies reported sufficient treatment detail for de novo MPAL classified according to the European Group for Immunological Characterization of Acute Leukemias (EGIL) or World Health Organization (WHO2008). Meta-analyses were performed for the endpoints of complete remission (CR) and overall survival (OS). A compiled case series for multivariable analysis was established from patients with data from time of diagnosis.
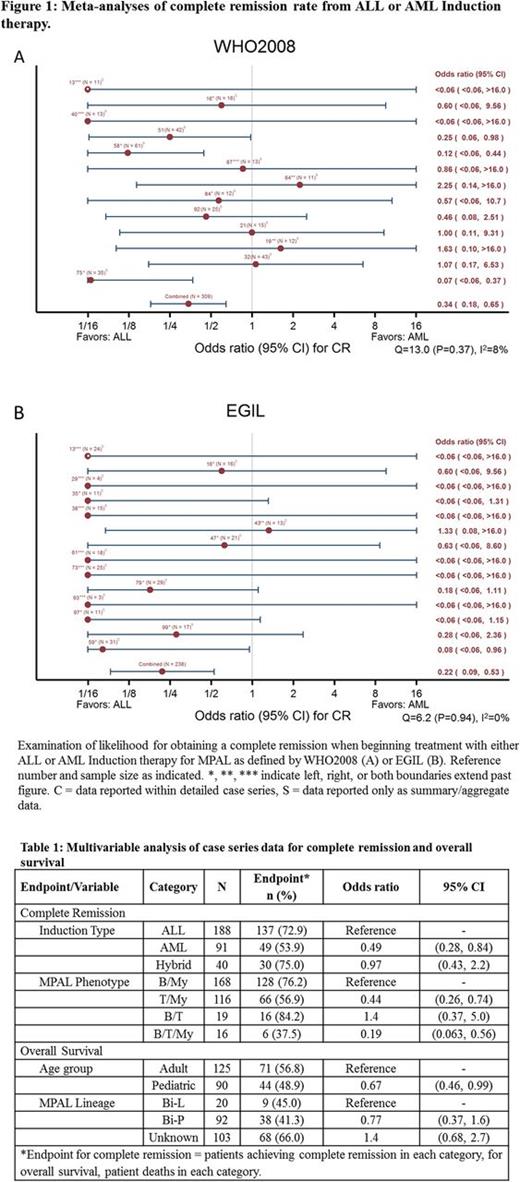
We identified 92 reports meeting criteria, resulting in 1,265 unique patients included in at least one quantitative analysis. Using either definition of MPAL, meta-analyses revealed that AML Induction was less likely to achieve a CR as compared to ALL regimens, (WHO2008 Odds Ratio [OR] = 0.34, 95% Confidence interval [95%CI] 0.18-0.65; EGIL, OR=0.22, 95%CI 0.09-0.53). Multivariable analysis of the compiled case-series supported poorer efficacy for AML Induction (Table 1). Meta-analyses found better OS with ALL therapy (WHO2008 OR=0.48, 95%CI 026-0.89; EGIL, OR=0.45, 95%CI 0.22-0.93) but multivariable analysis of the compiled case series showed only adult age as predictive of lower survival (Table 1). MPAL definition did not impact trends within each endpoint. Examination of presenting features of MPAL revealed hyperleukocytosis and central nervous system involvement to be uncommon (<25%). For either classification system of MPAL, ALL-directed therapy is associated with higher initial remission rates and is at least equivalent to more intensive AML therapy for long-term survival. Prospective trials are urgently needed to establish a uniform approach to this heterogeneous disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal